Indiana Doctors First To Use Clot Removal Device
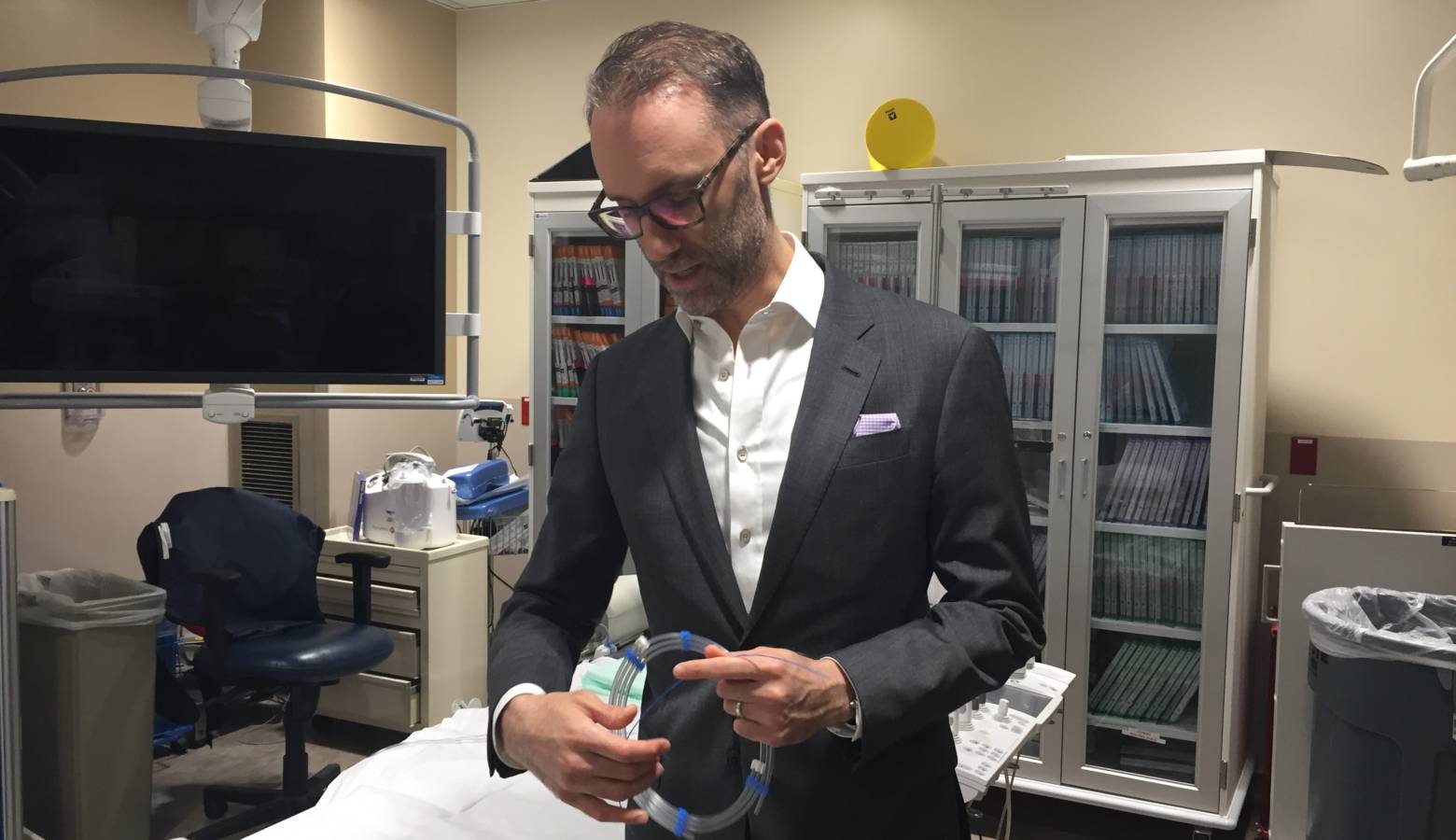
Indiana doctors are some of the first in the country to use a new tool that increases the ability to extract clots from the head which can reduce the damage from a stroke. Indiana Public Broadcasting’s Jill Sheridan talked to Goodman Campbell Brain and Spine Surgeon Dr. Dan Sahlein at a St. Vincent hospital in Indianapolis about a newly approved device called the Embotrap II that can change a stroke patients outcome for the better.
Sheridan: Doctor can you explain how you and your colleagues became some of the first in the nation to be using this device.
Sahlein: We have one of the largest stroke practices in the country. And when I say stroke practice, I mean we’re the physicians who use catheters, long skinny plastic tubes, thread them up through the artery in the leg to an artery in the brain and mechanically extract a blood clot or a little plug that’s blocking an artery in the head in the setting of an acute ischemic stroke. A stoke caused by blockage of an artery in the head; where the brain on the distal of that blockage is slowly or sometimes rapidly dying.
So when this new tool was being introduced, they came to us first and asked us if we’d like to be the first users and we accepted.
Sheridan: What did you think when you first used this new tool?
Sahlein: The tool is the latest offering in a broader category of tools called stent retrievers. Essentially it’s an expandable stent connected to a wire that acts a little bit like a rake. The stent is compressed into a very small catheter, we thread that catheter into the head, past the clot or into the clot. We then push this tool through the catheter then pull it back allowing the stent to expand into the clot and it gets enmeshed in the clot and then acts as a rake to extract the clot from the blocked vessel in the head.
The Embotrap is third of this type of tool to be introduced in the market in the U.S. and as a broad category the tools have really revolutionized the care that we can provide patients who are having acute ischemic stroke.
Sheridan: So there’s something you can do if you’re experiencing a stroke and having those symptoms. Now with this new wave of technology and devices, there is a lot you guys can do.
Sahlein: The first thing that is probably the most important component of all this is that patients get to the hospital very, very quickly. Essentially we are racing the clock, what we say is ‘time is brain’ meaning that once an artery is blocked, the brain on the other side of that blockage is slowly or sometimes rapidly dying. The brain on the other side of the blockage is initially in what we called a stunned by salvageable state.
What we then do is race them to the hospital along with a team of technologists, nurses and anesthesiologists, get the patient to our lab as quickly as possible, and do this procedure. To go into the artery in the leg, thread the catheter and mechanically extract that clot. The critical piece of all of that is to get the patient to the hospital quickly.
So we use the acronym FAST. F standing for if you see someone with facial asymmetry. A is for arms, ask someone to lift an arm and if that is asymmetric, they can’t lift an arm. The S stands for speech, meaning that if there is any abnormality with speech you need to get them to a hospital. And the T stands for time.
Sheridan: What personally have you experienced in terms of results with a device like this?
Sahlein: Many but not all of our results, but many of them are really astonishing. Patients come into the hospital with the inability to move the right side of their body, inability to speak, to understand language and we have patients that literally walk out of the hospital two days later.
The difference is really astonishing, on the one hand you’re talking about someone who may neurologically devastated and on the other hand you’re talking about someone who goes onto to live a completely normal, functional life.
